Egas Moniz
Article

Controversial Psychosurgery Resulted in a Nobel Prize
by Bengt Jansson*
This article was published on 29 October 1998.
Summary
In 1936, the Portuguese neurologist Egas Moniz introduced a surgical operation, prefrontal leukotomy, which after an initial period came to be used particularly in the treatment of schizophrenia. The operation, later called lobotomy, consisted in incisions that destroyed connections between the prefrontal region and other parts of the brain.
At that time there did not exist any effective treatment whatsoever for schizophrenia, and the leukotomy managed at least to make life more endurable for the patients and their surroundings. The treatment became rather popular in many countries all over the world and Moniz received the Nobel Prize in 1949.
However, by this time the treatment had had its most successful period and in 1952 the first drug with a definite effect on schizophrenia was introduced, chlorpromazine, our first neuroleptic drug. Since about 1960 lobotomy, with a strongly modified technique (more discrete incisions), has been used only when there are very special indications such as in severe anxiety, and compulsive syndromes which have proved to be resistant to other forms of therapy. Perhaps about five operations a year are now being performed in Sweden.
However, I see no reason for indignation at what was done in the 1940s as at that time there were no other alternatives!
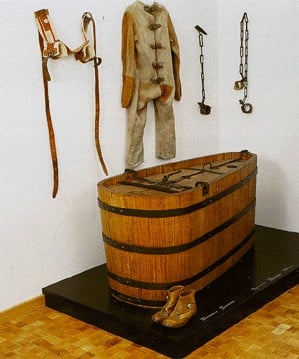
Chains, straitjacket, cell belt and covered bath tub (72 x 150 x 69 cm) for restraining raving patients, Burghölzli Hospital, Zurich.
Therapeutic Alternatives for Psychotic Patients Before the 1930s
As a rule therapeutic methods developed considerably later in psychiatry than in other medical fields. Violent patients, dangerous to their surroundings, sometimes had to be restrained or immersed in baths for long periods. Another alternative was heavy sedation with opiate derivatives or barbiturates. However, none of these treatments had long-term effects on psychotic patients.
It was not until the 1930s that Manfred Sakel in Vienna introduced hypoglycaemic coma, produced by injections of insulin, as a treatment for schizophrenia. At the same time the Hungarian Ladislav von Meduna started seizure therapy by intravenous injection of cardiazol (in depressive states), a therapy that was abandoned when in 1938 the Italians Cerletti and Bini introduced electric convulsive therapy, E.C.T., for severe mental states. This treatment was first used in schizophrenia, but severe depressive states very soon proved to be the main indication. Tranquilizers with more than a very short-lived sedative effect did not exist until 1952 when the Frenchmen Delay and Deniker introduced our first neuroleptic drug, the phenothiazine derivative chlorpromazine.
Introduction of Prefrontal Leukotomy*
Cerebral surgery had been tried in a few psychiatric cases as early as 1891 and 1910, particularly patients with manic-depressive psychosis. These trials did not attract much attention, but at a neurology conference in London in 1935, at which the Portuguese neurologist Egas Moniz participated, Jacobsen & Fulton presented data from operations on two chimpanzees which, after a leukotomy, managed to make mistakes without becoming aggressive, something which they had not managed to do before. Many people have considered this information to have instigated Moniz’s “bold step” in November 1935. In 1936 Moniz published his first report on prefrontal leukotomy.
One reason why Moniz’s operations gained better acceptance than the earlier trials mentioned above was evidently the fact that he was internationally respected for having developed cerebral angiography. Moniz’s first twenty cases all survived and did not develop any serious morbidity. The leukotomy soon achieved a good reputation in, among other countries, Brazil, Italy and the United States. Moniz strongly believed that the potential benefits of surgical lesions in the frontal lobes, even allowing for some behavioral and personality deterioration, outweighed the debilitating effects of severe psychiatric illness.

Leucotome.
Refined Surgical Techniques
Moniz, working together with the neurosurgeon Almeida Lima, first injected alcohol as a sclerosing agent into the white matter of the frontal lobes. Moniz soon refined his technique by designing a “leucotome,” an instrument with a retractable wire loop and later replaced with a steel band, which he used to cut six cores in the white matter of each hemisphere. For twenty patients in a first series, and eighteen in a second, the results were considered rather acceptable by Moniz in 1937, although he concluded that deteriorated patients did not benefit much from the operation. Of the 18 patients in the second group (all schizophrenic), three were characterized as almost cured and another two also had become much better. Moniz’s conclusion was this: “Prefrontal leukotomy is a simple operation, always safe, which may prove to be an effective surgical treatment in certain cases of mental disorder.”

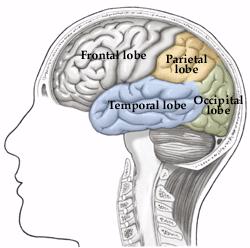
The blue spots indicate the areas operated on.
Among those who followed Moniz’s lead, none was more prominent than the neurologist and neurosurgeon team of Walter Freeman and James Watts in the United States. Freeman and Watts first used Moniz’s leucotome technique, but they soon developed a procedure designed to more completely ablate the white matter tracts to and from the prefrontal lobes. Freeman and Watts performed about 600 operations with this “closed procedure,” which became known as the standard prefrontal lobotomy of Freeman and Watts. The first “open operation” was performed by Lyerly in 1937 who, using a superior approach to each frontal lobe with the aid of a specially lit speculum, attempted to separate the white fibers under direct vision. This method became the standard procedure in the United States as the open method was considered to reduce the main complication of psychosurgery, haemorrhage of the anterior cerebral artery.
Side Effects on Personality
Negative effects on personality were observed as early as the end of the 1930s. In 1948, Swedish professor of forensic psychiatry Gösta Rylander, reported a mother as saying: “She is my daughter but yet a different person. She is with me in body but her soul is in some way lost.” Hoffman (1949) writes: “these patients are not only no longer distressed by their mental conflicts but also seem to have little capacity for any emotional experiences – pleasurable or otherwise. They are described by the nurses and the doctors, over and over, as dull, apathetic, listless, without drive or initiative, flat, lethargic, placid and unconcerned, childlike, docile, needing pushing, passive, lacking in spontaneity, without aim or purpose, preoccupied and dependent.”
Who Were Operated On?
Initially operations were performed on a majority of patients with affective disorders, i.e. various types of depression, such as involutional depression, agitated depression and so on. Very few psychiatrists remember this because E.C.T. (electric convulsive therapy) had already been introduced in 1938 and quickly proved to be a very effective treatment for depressive states. Other groups of patients were those with severe obsessive-compulsive and hypochondriac states. As a rule, severity was a more important factor than diagnosis, i.e. consideration was taken to suicidality and dangerousness, among other things.
A few patients suffering from schizophrenia were operated on at the end of the 1930s, but neither Moniz’s original seven patients nor any of those 12 schizophrenic patients from Freeman & Watts´ first 80 cases showed any marked improvement. Freeman based his opinion quite early on that if schizophrenic patients are to be operated, it should be done early before they have become apathetic or have deteriorated, because such patients “behaved the same with or without their frontal lobes” (Swayze 1995). This opinion became more and more dominant (Kalinowsky & Scarff, 1948). In other words the first year of illness should be used to try all the other somatic therapies. At a conference in 1953, it was shown that mortality varied between 0.8% and 2.5%. At the same time, approximately 10% of operated patients were known to have some problems with epilepsy.
Why Was Psychosurgery so Popular in the 1940s?
Swayze (1995), whose paper is strongly recommended for reading (see reference), mentions some important contributory factors. First, there were no alternative therapies available for chronically institutionalized patients. Second, during and following World War II there was an alarming increase in the number of admissions to psychiatric institutions in the United States. For example, there were 100,000 new admissions to mental institutions and only 67,000 discharges in 1943, and in 1946 nearly one-half of the public hospital beds were devoted to the mentally ill (Menninger 1948). Third, prior to 1930, patients continuously hospitalized for 15 years with a diagnosis of manic-depression had a 18% mortality rate due to tuberculosis and other infectious diseases. Thus, the importance of discharging patients from the state institutions was apparent. Another factor, according to many doctors, was that a long stay in a mental institution in itself contributed to the fact that many patients became apathetic.
Were the Patients Cured?
A survey of all patients who underwent leukotomy in England and Wales from 1942 to 1954 (Tooth et al 1961) documented 10,365 single leukotomy operations. An additional 762 patients underwent more than one operation. A follow-up study covering 9,284 of the above mentioned patients showed that 41% had recovered or were greatly improved while 28% were minimally improved, 25% showed no change, 2% had become worse and 4% had died. Not surprisingly, patients with an affective disorder showed the best prognosis with 63% recovered compared to 30% among schizophrenic patients.
In the United States approximately 10,000 operations had been performed by August 1949. After 1954 the number of operations steadily decreased. As there were no alternative therapies for severe mental disorders, psychoses in the 1930s, it is not surprising that lobotomy was quickly accepted as a therapy for chronic schizophrenic psychoses, even if it seems a bit strange that lobotomy initially was tried with affective disorders. Lobotomy is an ethically dubious treatment if carried out against the patient´s wishes, but this is always a difficult question in severely psychotic patients who totally lack insight about their illness – what is it exactly that such a patient wants? Historically, it is easy to understand that psychosurgery was considered as a therapeutic advance. Today, it is easy to hold a negative opinion about the use of lobotomy and consider it very strange that Moniz was awarded the Nobel Prize. However, I agree with Swayze (1995) who has written: “If we learn nothing else from that era, it should be recognized that more rigorous, prospective long-term studies of psychiatric outcome are essential to assess the long-term outcomes of our treatment methods.”
Development of Alternative Methods
The development of neuroleptics, which started with chlorpromazine in 1952, very soon made lobotomy uninteresting in the treatment of schizophrenia, and the number of lobotomies in schizophrenia dropped dramatically after about 1960. During the 1970s a refined computed tomography-based stereotactic technique was developed making it possible to make selective lesions of specific fiber systems. The main target area is the limbic system which is closely related to emotions. The most important procedure is bilateral anterior capsulotomy (in the United States also cingulotomy), and the indications have changed to chronic anxiety – and obsessive compulsive syndromes which have shown themselves resistant to other treatments. Anxiety disappears first, but the obsessive symptoms gradually also diminish when they are not maintained by anxiety. In Sweden we perform about 5 such operations a year.
Chlorpromazine.
Did Moniz Deserve the Nobel Prize?
Moniz, who was born in 1874, was shot in the leg by a patient and had to spend the rest of his life in a wheel chair (he died in 1955). Moniz had problems with his hand and did not very often hold the knife himself. However, there is no doubt that it really was Moniz who initiated and managed to inspire enthusiasm for the importance of prefrontal leukotomy in the treatment of certain psychoses. The more sophisticated surgical methods, however, were developed by other people, primarily by Freeman and Watts but also by Lyerly-Poppen, Strecker and others. Moniz’s main interests were evidently encephalography, and cerebral arteriography. Already in the 1920s Moniz succeeded in making cerebral arteriographies possible by injections of a contrast agent containing iodine, an invention which made it possible to diagnose tumors and vascular deformities. Actually, I think there is no doubt that Moniz deserved the Nobel Prize.
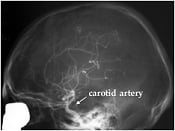
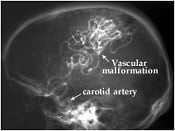
X-ray examination of brain vessels using the method – cerebral angiography – introduced by Moniz. A radio-opaque contrast medium has been injected into one of four neck vessels (carotid artery) supplying the brain. Normal case (left). A case of vascular malformation situated in the parietal (mid superior) part of the brain and fed by an enlarged artery (right).
Moniz’s life history contains a few surprising details. He grew up and was educated in Coimbra, but after having been professor there and also professor of neurology in Lisbon in 1911-14, he devoted some years to business and politics. Moniz became ambassador to Madrid in 1918 and in 1918-19 was minister for foreign affairs before returning to the Institute of Neurology in Lisbon.
Glossary
Affective disorders – all states where the patient’s mood is higher (manic or hypomanic states) or lower than normal, that is, various kinds of depression, for instance, involutional depression in old people with signs of ageing. (Manic-depressive psychosis is an older term for the same kind of disorders).
Cerebral angiography – an X-ray investigation of the blood vessels of the brain. The blood vessels are made visible by injecting a dye that is opaque to X-rays.
Cingulotomy and bilateral anterior capsulotomy – are methods used to destroy connections between cortical areas and basal ganglia, areas which have shown signs of hypermetabolism in tomographies. The operations may be accomplished by thermic coagulation with high frequency electric current or gamma radiation. In the former method electrodes are conveyed through two bore-holes, and the latter method is totally unbloody.
Electric convulsive therapy (E.C.T.) – is the most efficient treatment of severe depressions. A short electric stimulation results in seizures which last for about 30 seconds. Repeated five to eight times, 3 times a week, this will as a rule make the patient healthy again without any side effects, except for minor memory disturbances which disappear within 3-4 weeks.
Encephalography – any of various methods for recording the structure of the brain or the activity of the brain cells.
Hypoglycemic – a state in which blood glucose level is below normal.
Leukotomy/Lobotomy – leukotomy is the surgical operation of interrupting the pathways of white nerve fibers within the brain. Lobotomy was the name given to a prefrontal leukotomy in which the nerve fibers connecting the frontal lobe with other parts of the brain were cut.
Limbic system – situated in the temporal lobe of the brain, is a center of vegetative functions, emotional experience, behavior and consolidation of memories.
Neuroleptics – which were introduced with chlorpromazine in 1952, are the most effective drugs in the treatment of psychotic symptoms (hallucinations, delusions, so-called “positive” symptoms) in schizophrenia. Many of them, but not all, also have sedative properties.
Obsessive-compulsive states – are conditions in which the patient sometimes may be very incapacitated by intensive thoughts he can not get rid of (obsessions), or ridiculous, meaningless things he feels compelled to do over and over again in order to hinder his anxiety level from increasing to an intolerable level (compulsions).
Prefrontal (lobe) – the area of the brain at the very front of each cerebral hemisphere. This area is concerned with emotion, memory, learning, and social behaviour.
Psychoses – are the most severe mental disorders, that is, schizophrenia, affective psychoses and also severe mental states often with confusional symptoms produced by toxic agents.
Schizophrenia – a psychotic condition, is the most severe psychiatric disorder. There are various subtypes, but symptoms like hallucinations, paranoid reactions and a reduced emotional capacity (and ability to relate to other people) and, sometimes, even isolation in an autistic state are characteristic. Until the introduction of neuroleptics in 1952, a majority of beds in our mental hospitals were used by schizophrenics, many of them from the age of 20-30 until death. Thanks to neuroleptics, most schizophrenic patients can take care of themselves outside hospitals, but very few become totally healthy. Most of them have residual symptoms which often make it difficult for them to work full-time, at least in qualified professions.
Stereotactic – a stereotactic surgical procedure is one in which a deep-seated area of the brain is operated upon after its position has been established with great accuracy by three-dimensional measurements.
Tomography – the scanning of a particular part of the body using X-rays or ultrasound. Computerized tomography (CT) scan is an X-ray procedure in which a computer draws a map from the measured densities of the brain. This method produces a three-dimensional representation of the brain
Tranquillizers – are drugs with a sedative effect enabling an anxious patient to relax. Some of these drugs are neuroleptics, whereas others only have a relaxation effect of a rather short duration, for instance, benzodiazepines.
References
Hoffman, JL: Clinical observations concerning schizophrenic patients treated by prefrontal leukotomy. N. Engl. J. Med. 1949, 241:233-236.
Kalinowsky, LB and Scarff, JE: The selection of psychiatric cases for prefrontal lobotomy. Am. J. Psychiatry 1948, 105:81-85.
Menninger, WC: Facts and statistics of significance for psychiatry. Bull. Menninger Clin. 1948, 12:1-25.
Swayze II, VW: Frontal leukotomy and related psychosurgical procedures in the era before antipsychotics (1935-1954): A historical overview. Am. J. Psychiatry 1995, 152 (4):505-515.
Tooth GC, and Newton, MP: Leukotomy in England and Wales 1942-1954. London, Her Majesty’s Stationary Office, 1961.
* Bengt Jansson, born 1932. M.D. 1956, Ph.D. 1964 at Göteborg University, Sweden (Post-Partum Psychoses). Since 1976 Professor of Psychiatry at Karolinska Institutet, Sweden. Member of the Medical Nobel Assembly, 1976-97. Main research interest in psychiatry since many years: Transcultural Psychiatry.
First published 29 October 1998
Nobel Prizes and laureates
Six prizes were awarded for achievements that have conferred the greatest benefit to humankind. The 14 laureates' work and discoveries range from quantum tunnelling to promoting democratic rights.
See them all presented here.
