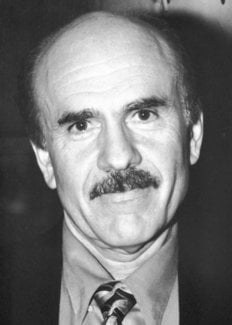
Louis J. Ignarro
Biographical
The first two decades of my life were spent in the New York City area, where the families of both my parents had settled in the 1920s after immigrating from Italy. My father had been a ship builder in Naples but my mother was still a young child when she came from Sicily. They met for the first time in Brooklyn, New York in the 1930s, were married, and then moved to the nearby coastal city of Long Beach. I was born on May 31, 1941 in Brooklyn and my brother, Angelo, followed on January 10, 1944. My father worked as a carpenter, whereas my mother elected to bring up her two sons at home.
Long Beach was a beautiful town, about 25 miles east of New York City located on the south shore of Long Island. We had a lovely home within walking distance of the beach along the Atlantic ocean. I can still recall walking to the beach and going for a swim nearly every day in the summer. My greatest joy each morning was building gigantic sand castles using dripping sand wetted by the incoming tide. All my friends believed and predicted that I would grow up to become an architect or engineer. This view was reinforced by my eagerness even as a young child to disassemble anything I could find and put it back together again. The joy of discovering that I could actually get the object to function again was quite rewarding and satisfying. But my greatest joy came when I was 8 years old. To my surprise and delight, mother and father finally responded favorably to my relentless request to have a chemistry set, and bought me one. I can recall vividly following every step of every experiment and becoming overjoyed at the success of each one. This was much more fun than building sand castles on the beach. My inquisitiveness drove me to the library to study more applied aspects of chemistry. Soon after completing dozens of additional experiments and going through several larger chemistry sets, I realized that what I really wanted to accomplish was to build a bomb and to send up a rocket. After about one year of experiments, I finally achieved those goals, albeit at the expense of numerous horrified reactions from the neighbors.
My interest in chemistry remained strong at Central Grade School and Long Beach High School, which led me to apply to Columbia University in New York City to study chemistry and pharmacy. I was especially pleased when I learned that I had been accepted to the freshman class at Columbia. I wanted to attend a university that was within commuting distance of home because I did not want to leave my family and friends in Long Beach. During my high school years I had developed a great interest in playing ball and racing cars, and I did not want that to come to an end, at least not just yet. My favorite sport was one-on-one stickball, the New York City sport of sports, where a “bouncy” rubber ball is thrown by the opponent pitcher against a brick or cement wall on which is drawn a “strike zone”. The batter uses a stick conveniently detached from a suitable broom or mop to hit the fast pitched ball. When I was not playing stickball I was building and racing cars at the West Hampton Drag Raceway. I guess I could never get away from taking things apart and putting them back together again. Indeed, I spent many long hours thinking about whether I should study chemistry or open up my own drag racing shop out on Long Island. Well, chemistry it was. I took dozens of chemistry courses, but a course in pharmacology, although poorly taught, really caught my attention. I studied the subject well beyond the course requirements and tried to hang around the pharmacology laboratories as often as I could. The result of this was my application to graduate school in pharmacology upon graduation from Columbia University in 1962.
I was delighted to be admitted to the pharmacology program at the University of Minnesota in Minneapolis, which was considered to be one of the best departments of pharmacology in the nation at that time. Actually, I had applied to the University of Wisconsin in Madison, where the department was located when I first applied. But for one reason or another, the entire department was relocated from Madison to Minneapolis just after I had been accepted in Madison. A bit confused, I reported to Minneapolis in September of 1962 to study pharmacology. At first, things were difficult for me because I had left my family, friends, stickball, racing cars and the beach behind. And then things got even worse when I experienced my first winter season of -40°F with winds of 30 mph. But I survived my first winter and went on to enjoy the upper midwest and the “Big Ten” college football games.
My studies in graduate school involved developing a better understanding of why and how neurons of the sympathetic nervous system innervate the heart and produce and release norepinephrine. I spent three of the most intense years of my life in the laboratory, where I was determined to unravel every bit of information possible within the time frame allotted to me to satisfy the research requirements for the PhD degree in pharmacology. My research was different from most in that it required, in addition to pharmacology, a great deal of knowledge in several other distinct disciplines such as physiology, biochemistry and anatomy. My major, of course, was pharmacology and I selected cardiovascular physiology as my minor. But that was insufficient, so I took several additional courses in biochemistry and anatomy. The most demanding course I took was enzymology, taught by Paul Boyer, who was awarded the Nobel Prize in Chemistry last year (1997). I have not stopped using enzymology in my research since taking that course. My research turned out to be acceptable to my committee, chaired by the late Frederick E. Shideman, MD, PhD, who was also Chairman of the Department of Pharmacology at the University of Minnesota. He decided that I should write four separate manuscripts on my thesis research and that we should submit them to the Journal of Pharmacology and Experimental Therapeutics. The editors of the journal accepted all four papers and published them back-to-back in one issue of the journal, a feat never again repeated either by the journal or by me.
After Minneapolis, I accepted a postdoctoral position at the National Institutes of Health in the Laboratory of Chemical Pharmacology in the National Heart, Lung and Blood Institute. My mentor was Elwood Titus, a brilliant scientist who was able to mix chemistry and pharmacology with the greatest of ease. I tried to learn as much as I could from him in two years. Perhaps I tried a bit too hard. For example, he asked me to study the chemistry of beta adrenergic receptors and I decided that I was going to isolate, characterize and elucidate the chemical structure not only of beta but also of alpha adrenergic receptors, all in two years. Having published four consecutive papers in a distinguished journal on my first try, I thought that my research career was going to be a breeze. The N.I.H. proved to me that this was not going to be the case, and it was not. My work resulted in only one publication, but the agony of frustration caused me to mature quickly. The atmosphere of the N.I.H. was highly conducive to learning science and I had the opportunity to discuss my work and research in general with Bernard Brodie, Jim Gillette, Julius Axelrod and other distinguished scientists.
My first real job after my research training was with the drug industry. Geigy Pharmaceuticals recruited me in 1968 with an attractive package including the responsibility of heading the biochemical and antiinflammatory program. Although this was an entirely new research topic for me, I accepted the position because of the enormous responsibility that would suddenly be mine. The work was quite satisfying in that I became a part of a larger group whose efforts led to the development and marketing of a new nonsteroidal antiinflammatory drug (diclofenac). About half way through my career at Geigy, my daughter, Heather, was born. I recall that day vividly (January 10, 1970) because I had to rush my wife to the nearby hospital in the midst of a snow storm. But all turned out well and I found myself devoting a great deal of time to something other than my own research. With the birth of Heather came a move from a small apartment in Hartsdale to a much larger unit in Irvington on the Hudson. This was a lovely neighborhood in which to raise a child.
In addition to my work on drug development, Geigy allowed me the freedom to pursue basic research in biochemical pharmacology, which led to my interest in studying the relatively new cyclic nucleotide, cyclic GMP. Although I enjoyed my work at Geigy Pharmaceuticals, when the company merged with Ciba Pharmaceuticals I decided to try my hand at academic research and teaching. In January of 1973, I accepted the position of Assistant Professor of pharmacology at Tulane University School of Medicine in New Orleans. I chose to go to Tulane because I wanted to continue my research on cyclic GMP, and there was a young pharmacologist at Tulane with the same interest. We moved to New Orleans, where we bought our first home in Terrytown, an attractive nearby suburb.
My interest and motivation in studying the possible physiological significance of cyclic GMP grew and grew during my first two years at Tulane. Thanks to my own laboratory and those of other interested collaborators, we made many significant contributions to the field of cyclic GMP and cyclic nucleotide research in general. My early work with cyclic GMP involved leukocytes and the heart, but this eventually led to an interest in blood vessels. I recall reading an interesting paper by Ferid Murad‘s group in 1977, in which nitric oxide and various nitro compounds were shown to activate the cytosolic form of guanylate cyclase and to elevate cyclic GMP levels in various tissues. Nitroglycerin was one of those nitro compounds that Ferid had studied and speculated might release nitric oxide which then activated guanylate cyclase. It occurred to me that nitric oxide might account for the vascular smooth muscle relaxing action of nitroglycerin and that cyclic GMP might be the second messenger responsible for mediating the vasorelaxant effect of nitric oxide. In 1979 we published the first account of the capacity of nitric oxide to relax vascular smooth muscle. We purchased a small cylinder of nitric oxide gas, made a dilution in nitrogen (nitric oxide is very unstable in the presence of oxygen), and injected a fine stream of gas bubbles into an organ bath in which was mounted a strip of bovine coronary artery precontracted by addition of phenylephrine. The result was a rapid and profound relaxation of the coronary artery strip. This vasorelaxant effect of nitric oxide was blocked by addition of hemoglobin, which promotes oxidation of nitric oxide, and methylene blue, which had been known to inhibit guanylate cyclase. And so we knew right away that nitric oxide was probably responsible for the vasorelaxant effect of nitroglycerin and that cyclic GMP was the likely ultimate mediator of relaxation, just as Ferid Murad had predicted.
We wondered whether the platelet antiaggregatory action of certain nitrovasodilators could also be attributed to nitric oxide and cyclic GMP. A relatively straightforward experiment was conducted with human platelet-rich plasma, in which we examined the influence of added nitric oxide on ADP-induced platelet aggregation. The results were dramatic. Nitric oxide potently inhibited platelet aggregation and actually reversed aggregation once it had occurred. This effect was mediated by cyclic GMP. Thus, at least two biological actions of nitric oxide were clear from these early studies. Nitric oxide is a vasorelaxant and inhibitor of platelet aggregation, and both effects are mediated by cyclic GMP.
The next step was to elucidate the mechanism by which nitroglycerin is converted to nitric oxide by vascular smooth muscle. After reading nearly every paper in the field of organic nitrate esters and their vasodilator effects, I was motivated by the work of Phil Needleman, who showed that the vasodilator action of nitroglycerin and other organic nitrate esters was dependent somehow on the presence of thiols. A long and tedious series of experiments in my laboratory led to the discovery that thiols were required for the activation of guanylate cyclase by nitroglycerin and related nitrovasodilators. Interaction between thiols and nitro compounds led to the formation of intermediate S-nitrosothiols, which were chemically unstable and decomposed to liberate nitric oxide gas. Depletion of tissue thiols resulted in diminished vasorelaxation by nitroglycerin because nitric oxide could no longer be generated. Moreover, tolerance to the vasodilator action of nitroglycerin appeared to be due to thiol depletion, which could be reversed by adding back thiols in order to generate more nitric oxide. This work was published in 1981 in the Journal of Pharmacology and Experimental Therapeutics.
Having elucidated the mechanism of action of nitroglycerin as a vasodilator, the next step was to understand how nitric oxide activates guanylate cyclase. An elegant series of experiments was published in the late 1970s by Patricia Craven and Fred DeRubertis, showing that activation of guanylate cyclase by nitric oxide might require the presence of heme. This made sense to me because heme iron had long been known to have a high binding affinity for nitric oxide. Suppose guanylate cyclase had a heme prosthetic group that bound nitric oxide and somehow became activated to generate more cyclic GMP from GTP? In 1981 we set out to purify and characterize guanylate cyclase from bovine lung. A young biochemically trained postdoctoral fellow from Yale University, Mike Wolin, joined my laboratory to tackle this project. After an incredibly long and tedious series of experiments, each often lasting for 96 consecutive hours, we found the heme in purified guanylate cyclase. Subsequent experiments revealed that the presence of enzyme-bound heme was an absolute requirement for guanylate cyclase activation by nitric oxide. We went on to propose that nitric oxide reacts with heme iron to alter the configuration of the catalytic binding site for GTP and promote the conversion of GTP to cyclic GMP and pyrophosphate. In conducting these experiments, we discovered that the non-nitric oxide containing substance, protoporphyrin IX, activated heme-deficient guanylate cyclase by kinetic mechanisms that were indistinguishable from the mechanism by which nitric oxide activates heme-containing guanylate cyclase.
Although the above observations were exciting, they were also puzzling because it was unclear why mammalian cells were so sensitive to nitric oxide. Why do we have receptors for nitric oxide, an air pollutant and a metabolite of nitroglycerin? Was it possible that our own cells actually produced nitric oxide or nitroglycerin but we were unaware of it? In 1983, my laboratory set out to determine whether or not mammalian cells can produce either nitric oxide or a nitro compound that could be metabolized to nitric oxide. A separate project in the laboratory was to study endothelium-dependent vasorelaxation and to attempt to identify the mysterious “EDRF” (endothelium derived relaxing factor) discovered three years earlier by Robert Furchgott. Both research projects came together in 1984 when we suddenly realized that EDRF and nitric oxide possessed similar pharmacological and biochemical properties. EDRF and nitric oxide were both chemically unstable and both activated guanylate cyclase and elevated tissue levels of cyclic GMP. The cyclic GMP elevating and vasorelaxant effects of both EDRF and nitric oxide were inhibited by addition of methylene blue to organ chambers. These findings, reported in 1984, prompted me to ascertain whether EDRF, like nitric oxide, required bound heme on guanylate cyclase in order to activate the enzyme and stimulate cyclic GMP formation. I can recall vividly the positive results of the first experiment, and I knew we had it. EDRF must be nitric oxide. I first reported these findings in the summer of 1986 at a vascular conference held at the Mayo Clinic in Rochester, Minnesota. Unexpectedly, at least to me, my colleague Robert Furchgott presented his own evidence that EDRF might be nitric oxide. I presented additional evidence a few months later at the fall American Heart Association meeting in Dallas and at the spring FASEB meeting in Washington, DC in 1987. So now it was clear why nitric oxide is such a potent vasorelaxant. This small lipophilic chemical is produced by vascular endothelial cells and functions to decrease vascular smooth muscle tone and to inhibit platelet aggregation.
The frenzy and excitement of these times in the mid-1980s was stalled at times by my divorce and my decision to leave Tulane University and begin a new personal life and academic career at UCLA School of Medicine. I moved to Los Angeles in May of 1985 and bought a small home in Encino, just 12 miles from the UCLA campus. My daughter, Heather, joined me in 1988 and attended California State University at Northridge. As a result of witnessing her dad’s commitment to many long hours of research and teaching, Heather chose to major in radio, film and television. At first, her decision to shy away from a career in science concerned me, but then I realized how talented she was and how successful she would become.
The discovery that EDRF was nitric oxide led to an avalanche of studies that created an exciting new field in biological research. New physiological and pathophysiological roles for nitric oxide were being discovered on a weekly basis. In record time, several prominent laboratories elucidated the biochemical mechanisms involved in the synthesis of nitric oxide by various cell types. While studying the relaxant effects of nitric oxide on vascular and nonvascular smooth muscle from corpus cavernosum erectile tissue, we realized that the naturally occurring physiological neurotransmitter involved in the erectile response in mammals was unknown. John Garthwaite had just reported that nitric oxide was a neuro transmitter in the brain, and we wondered whether or not nitric oxide could be the neurotransmitter in the so called nonadrenergic noncholinergic neurons that were known to innervate the corpus cavernosum smooth muscle. After all, nitric oxide released from such nerves would be expected to diffuse into the nearby vascular and nonvascular smooth muscle and cause relaxation. Such an effect could account for the marked relaxation of both vascular and nonvascular smooth muscle that accompanies the erectile response and allows for the engorgement of blood in the sinusoidal or trabecular network of blood vessels in the corpus cavernosum. The first carefully designed experiment was successful. Electrical stimulation of strips of rabbit corpus cavernosum caused a transient but marked smooth muscle relaxation that was prevented by addition of a nitric oxide synthase inhibitor and enhanced by addition of a cyclic GMP phosphodiesterase inhibitor. Addition of authentic nitric oxide to organ chambers mimicked the effects of electrical stimulation. A subsequent experiment revealed that electrical stimulation results in the production of nitric oxide in the corpus cavernosum. Further studies using human tissue showed that patients with impotence suffer from an impaired nitric oxide cyclic GMP pathway in the erectile tissue, and this work laid the foundation for the development by others of a drug that proved to be effective for the treatment of impotency in humans. Sildenafil (ViagraR) promotes the erectile response by inhibiting a specific isoform of cyclic GMP phosphodiesterase and allowing cyclic GMP to accumulate when guanylate cyclase is activated by nitric oxide released from the nerves innervating the erectile tissue.
In the fall of 1994, I met Sharon Elizabeth Williams, a lovely and charming medical student here at UCLA. Sharon had been a nurse anesthetist for several years and then decided to obtain an M.D. degree in order to practice anesthesiology at a more professional level. After graduating from UCLA, Sharon moved to the east coast to begin her internship and residency at Johns Hopkins University. Shortly after her move, we started dating by long distance and were married in July of 1997. A year later, in the spring of 1998, Sharon transferred back to UCLA to continue her residency in anesthesiology. Finally, we were together. During the week we reside in an apartment adjacent to the UCLA campus in Westwood and we spend our weekends in my home in Malibu.
As a result of my work during the past decade, many investigators jumped in to extend our findings. This led to the development of close collaborations with numerous laboratories and the formation of close and genuine friendships in many different parts of the world. I treasure these friendships even more than the awards I have received for my research accomplishments. I also realize that these accomplishments would not have been possible without the interest, hard work, and commitment on the part of my technical assistants, graduate students, postdoctoral fellows, medical fellows, visiting scientists, research collaborators at home, and collaborators at other institutions.
Another rewarding development has been my discovery that I also have a real knack for and love of teaching what I know to medical and graduate students. I have consequently made teaching a regular part of my schedule since I came to UCLA and I cherish the Golden Apple teaching awards I have won from my classes. I trust that I have helped guide at least some of these young people toward careers that will be a blessing to them and to humanity. In my own case, the combination of biomedical research and teaching continues to provide me with an exciting and useful life, and I am exceedingly grateful.
This autobiography/biography was written at the time of the award and later published in the book series Les Prix Nobel/ Nobel Lectures/The Nobel Prizes. The information is sometimes updated with an addendum submitted by the Laureate.
Nobel Prizes and laureates
Six prizes were awarded for achievements that have conferred the greatest benefit to humankind. The 14 laureates' work and discoveries range from quantum tunnelling to promoting democratic rights.
See them all presented here.