
by Frank Fenner and Suzanne Cory
Medical research in Australia in the early 20th century
Although politically independent since 1901, in the 1920s Australia was still culturally, scientifically and industrially a dependency of the United Kingdom. The total population then was some 7 million and there were three medical schools, in Sydney, Melbourne and Adelaide. The few professors in each were overwhelmed with teaching responsibilities, and medical research was essentially a part-time activity. All medical graduates who aspired to do more than general practice, whether as physicians or surgeons or, for a very few, to do research, went to England for further training. Some of the best stayed: Howard Florey, Grafton Elliot Smith, Hugh Cairns, and Neil Hamilton Fairley.
The beginnings
The Walter and Eliza Hall Institute of Pathology and Medicine was founded in 1915 as a privately funded research institute associated with the Melbourne Hospital. Because of the First World War, it did not commence operations until 1920, with an English physician, Sydney Patterson, as Director, primarily as an adjunct to the pathological and bacteriological laboratories of the Melbourne Hospital. Having graduated in medicine at the University of Melbourne in 1922, Frank Macfarlane Burnet joined the staff in 1923 as pathological registrar, and became senior resident pathologist a few months later. In 1923 Patterson resigned to return to England, and in 1924 Charles Kellaway, a Melbourne graduate who had been working with Sir Henry Dale in London, arrived as the new Director.

C. H. Kellaway (on left), as new Director, being met in Melbourne by F. M. Burnet in 1924.
Copyright © Walter and Eliza Hall Institute
The Kellaway years (1924-1944)1,2
In 1918 Kellaway was discharged from the Australian Army while in London, and went to work with Sir Henry Dale at the National Institute of Medical Research. Enthused by this experience, when appointed to be Director of the Hall Institute in 1923 he wished to establish a tradition of full-time research in the biomedical sciences in Australia. He set up three departments; physiology and pharmacology, of which he took charge, biochemistry, and bacteriology. He appointed Henry Holden, from the University of Cambridge, to head biochemistry and Burnet to head the bacteriology department. However, cognizant of the importance of overseas experience, in 1925 Kellaway sent Burnet to London to work at the Lister Institute, where he worked on bacteriophages until 1927, and secured a PhD degree.
Hamilton Fairley, already a man of standing in tropical medicine, was available and worked with Kellaway for two years on hydatid disease and snake venoms. Harold Dew, later long-time Professor of Surgery at the University of Sydney, collaborated in the study of hydatid disease. Then, in 1929, came the Great Depression, and finances did not resume an upward trend until 1933-34. Kellaway himself made important contributions to the pharmacology of venoms of snakes, spiders and mussels.3 E.R. Trethewie, working with Kellaway, made pioneering discoveries of ‘slow-reacting substances’, later famous as leukotrienes. In 1937 Wilhelm Feldberg, already a famous pharmacologist, came via Hampstead as a refugee from Nazi Germany, but returned to London just before the outbreak of war. By 1939 the Institute had reached a peak of prosperity and productivity; by far the best medical research in Australia was being done there. Four of the small staff; Kellaway, Fairley, Feldberg and Burnet, were to become Fellows of the Royal Society. Since its establishment in 1915, the Institute had been housed in part of the old Melbourne Hospital, sharing with the clinical pathology department of the hospital three floors and a basement, without even a service lift. Now was the time to acquire new, custom-built laboratories, and the fact that the Melbourne Hospital was to move to new premises offered the opportunity, which Kellaway seized. The new building provided much better accommodation, with a floor each for each department, service rooms and an extensive basement for heavy equipment. The staff moved across in 1942.
 |
 |
| The premises occupied by the Walter and Eliza Hall Institute of Medical Research in the Melbourne Hospital, 1923-1942. | Laboratories of the Walter and Eliza Hall Institute in the new Royal Melbourne Hospital, 1942-1985. |
| Copyright © Walter and Eliza Hall Institute | |
The man who was to make the greatest contribution to the international stature of the Hall Institute, from that time until he retired in 1965, was Macfarlane Burnet. Returning to Melbourne in 1927, he concentrated on bacteriophage studies, making seminal discoveries in lysogeny and bacterial genetics.4 However, in January 1928 there was a disaster in the country town of Bundaberg, in Queensland, when 18 of 21 children who had received injections of a toxin-antitoxin mixture became ill within the next twelve hours and 12 died. Kellaway was appointed Chairman of a Royal Commission to investigate the fatalities, and Burnet was given responsibility for the laboratory investigations. Having shown that Staphylococcus aureus could be isolated from the fluid in the bottle and lesions of survivors, Burnet commenced a study of staphylococcal alpha toxin and on staphylococcal bacteriophages. This event was significant in the history of the Hall Institute for two reasons. Firstly, the effective work of Kellaway and his staff on a matter of great public interest impressed the name of the Walter and Eliza Hall Institute and the significance of medical research on the Australian public. Secondly, almost as an aside to his study of the staphylococcal toxin, Burnet made observations of the antibody response of rabbits to injections of the toxoid. He observed the small and slow response to the first injection and the immediate and rapid rise in the antitoxin level after the second injection. He interpreted this as indicating that something was duplicating itself every twelve hours or so to produce the antibody. His paper on these results and their implications was rejected by the British journal to which it had been sent, and this, his first rejection, stimulated him to collect further information on the production of antibodies and publish all this data in an un-refereed Hall Institute monograph, The Production of Antibodies.5 Data on the primary and secondary responses also figure prominently in the second edition; for Burnet this was overwhelming evidence that the then fashionable “instructive” hypothesis of antibody production could not be correct. It was in this second edition that he made theoretical observations on immunological tolerance for which he was to share the Nobel Prize with Peter Medawar in 1960.
Throughout his life Burnet felt a strong obligation to respond to local outbreaks of infectious diseases, especially if a viral etiology was suspected. In the 1920s and 1930s poliomyelitis epidemics were a recurring problem in Melbourne, and in 1931 Burnet isolated a strain of poliovirus from a case which he showed was serologically unrelated to the Flexner strain; this was the first indication that there was more than one serotype of poliovirus. He returned to the study of polioviruses in 1939, following a very severe outbreak of poliomyelitis in Australia. His major contributions then were to show that cynomolgus monkeys could be infected orally and that poliovirus could be recovered from pharyngeal tissue and the mesenteric lymph nodes. He also carried out one of his very few experiments using tissue culture, demonstrating that poliovirus would multiply in cultured human foetal intestinal and buccal tissues.
In 1932 Burnet travelled again to London, at the invitation of Sir Henry Dale, who had secured funds from the Rockefeller Foundation to develop laboratory studies on animal viruses. He joined C. H. Andrewes and his colleagues at the National Institute of Medical Research, but proceeded to work quite independently. His main effort was converting Goodpasture’s method of growing vaccinia virus on the chorioallantoic membrane of the developing egg to provide a method of titration of viral infectivity and anti-viral antibodies, for several different viruses. By this time he had developed a pattern of publishing a long review article after he had published a number of research articles on a particular subject; he had done this for the bacteriophage work, for his speculations about the production of antibodies, and now for the use of the chick embryo in virus research.6 Also, while at Mill Hill Laidlaw’s comment “The ferrets are sneezing,” which signalled the first isolation of influenza virus from a human case, made a deep impression. Influenza virus was to be the centre-piece of his experimental research for many years, from 1940 to 1957.
In 1934 Burnet came back to the Hall Institute. He rounded off his work on bacteriophages and continued to study the growth of different viruses on the chorioallantoic membrane. Following his principle of working on infectious diseases that had impinged on the Australian public and might have a viral etiology, he undertook studies on psittacosis and a novel disease that had been in Queensland abattoir workers, Q (for query) fever. The studies on psittacosis brought home to Burnet the importance of latent infections in diseases of vertebrates as well as in bacteria, in which he had long before recognized the nature of lysogeny. This work with psittacosis activated his interest in the ecology of infectious diseases, which he developed in his first semi-popular book Biological Aspects of Infectious Diseases,7 written “from the point of view of a biologist as much interested in how the parasite species survives as in how the host resists it”. Under a different title, it went through three further editions, was translated into German, Italian, Japanese and Spanish, and had a major impact on the thinking of many microbiologists and biochemists world wide.
Q fever had been recognized in 1935 as a typhoid-like disease of abattoir workers from which no bacteria could be cultivated, but which could be passed to guinea pigs. It was presumed to be due to a virus, and as Australia’s only recognized virologist, material from guinea pigs was sent down to him.8 On histological examination of tissues from an infected mouse he noticed a “vague herringbone pattern” which recalled what he had seen in psittacosis and had read about for rickettsiae, and using Castaneda’s stain he had no doubt that the organism was a rickettsia. It was subsequently named Coxiella burnetii.
He made important contributions to two other viral diseases, herpes virus infections and ectromelia, showing that aphthous stomatitis in infants was often due to infection with herpes simplex virus and that the virus then went into a latent phase, recurrent facial herpes occurring later in life, in the presence of high titres of antibody. Then, after a colleague had shown that vaccinia virus produced a unique type of haemagglutination, Burnet went on to demonstrate that ectromelia virus showed the same type of haemagglutination and that ectromelia and vaccinia viruses were cross-protective in animals.
From about 1940 Burnet’s main interest in virology was influenza virus.9 He showed that influenza virus could be isolated from human cases by inoculation of throat washings into the amniotic sac, and a year later that virus isolated in this way could be quickly adapted to grow in the allantoic sac. This provided a method for large-scale production of virus for the manufacture of vaccines that is still in use. Exploration of the mechanism provided his first essay into influenza virus genetics, the demonstration that the “O-D change” which made possible growth in the allantoic sac was due to a mutation, a phenomenon that had not been demonstrated with animal viruses at that time.
With the onset of the Second World War Kellaway became scientific liaison officer on the staff of the Director General of the Australian Army Medical Service. As Assistant Director, Burnet now took on much of the administrative work of the Institute. Remembering the terrible scourge of influenza after the First World War, he decided that his war effort would be to develop a live virus vaccine. This got through what we would now call phase 1 and phase 2 trials, and he was set to carry out a trial on 20,000 troops when word came that the US Army was producing a killed virus vaccine. Further trials were abandoned. In 1944, as the end of the war approached, Kellaway accepted an invitation to become head of the research laboratories of Wellcome Foundation Ltd. in London. In the same year, Burnet made his first trip to the United States, to give the Dunham lectures at Harvard University. Before he left, Kellaway told him of his impending departure and said that he would strongly recommend that the Board should appoint him as Director, a position to which he was appointed later in 1944.
Burnet as director of the Hall Institute, 1944-1965
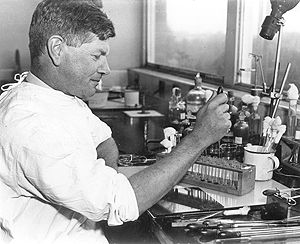
F.M. Burnet in the laboratory in the early 1950’s. He was experimenting on influenza virus genetics, using the developing hen’s egg.
Copyright © Walter and Eliza Hall Institute
Burnet was greatly impressed by what he had seen at Harvard University, and set out to achieve something of that pattern in Melbourne. Conscious that “medical research” was seen by the public as something associated with curative medicine, his first innovation was a Clinical Research Unit, to which he appointed Ian Wood, a leading gastroenterologist. Then, seeing that modern science required larger teams than the two or three persons that had worked in various departments of the Hall Institute before the War, he decided to concentrate all laboratory work in the Institute on virology, and with the discovery of influenza virus haemagglutination in the United States in 1941, on influenza virus. Holden was deputed to set up new biophysical equipment, Alfred Gottschalk, a highly skilled yeast biochemist who had come as a refugee from Germany in 1939, was called on to unravel the enzymology of the “receptor-destroying factor”, as neuraminidase was called, and in 1948 a young Sydney graduate in biochemistry, Gordon Ada, was appointed to back up the biochemists. Arising out of Burnet’s discovery that ectromelia virus was closely related to vaccinia and smallpox viruses, Frank Fenner was appointed in 1947 to study the experimental epidemiology of ectromelia. He showed that it caused a rash in mice; these studies led much later to his involvement in the WHO smallpox eradication campaign and the award of the 1988 Japan Prize. Other appointments over the next few years included Gray Anderson, Eric French, Eric Saint, Donald McLean and Donald Metcalf; Stephen Fazekas came in 1947 as a refugee from Hungary. All were to become distinguished in various fields in Australia or overseas. Another feature that demonstrated the international stature that the Hall Institute had then attained was the number of overseas visitors who came as postdocs or on a sabbatical. Young men whose names were later known internationally included Bernard Briody and Carleton Gajdusek (who discovered kuru at this time, for which he was awarded the Nobel Prize in 1976) from the USA, and John Cairns, Alick Isaacs (whose early death deprived him of adequate recognition for the discovery of interferon), and Barrie Marmion from England.
Burnet’s team unravelled the function of influenza virus neuraminidase and Ada demonstrated that the influenza virus genome was RNA, while Burnet himself concentrated on influenza virus genetics. After clarifying the mutational nature of the “O-D change,” he demonstrated that when cells were mixedly infected with strains with different properties they recombined readily. Indeed, they recombined with such high frequency that other scientists, believing that what happened with bacteriophages must happen with all other viruses, did not believe it. Always ready to speculate, Burnet himself suggested that perhaps the genome of influenza virus “may fracture and the fragments replicate themselves independently”. Some ten years later it was demonstrated that the influenza virus genome was indeed fragmented, and that high frequency recombination was indeed due to reassortment of these fragments. During this period he further consolidated his reputation as one of the world’s greatest virologists by the publication of the first comprehensive book on animal viruses.10
Burnet was curiously conservative in not taking up tissue culture as a virological tool, and was hostile to the ideas of molecular biology. In 1957 he had published a short paper on the clonal selection theory of antibody production, later elaborated as a major book.11 He felt that he had done as much as he could in virology, and he wanted to devote the last seven years of his life as Director to the implications of this theory, for which he had been groping ever since his first speculations about the significance of the secondary response in 1929, and he abruptly switched the focus of the Institute to immunology. A few years later his hunch that immunology would be a more “rewarding” field than virology was confirmed by the award of the 1960 Nobel Prize to him and Peter Medawar for the discovery of immunological tolerance, a discovery in immunology of minor importance compared with the clonal selection theory.
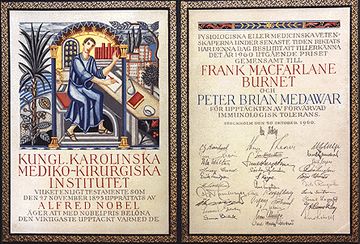 |
| The diploma of the 1960 Nobel Prize in Physiology or Medicine for F. M. Burnet and P. B. Medawar. Copyright © Walter and Eliza Hall Institute |
Nossal’s term as Director, 1965-1996 12

F.M. Burnet with PhD student G.J.V. Nossal, who became Director of the Institute in 1965, at the age of 34.
Copyright © Walter and Eliza Hall Institute
Burnet stayed on for one year after his nominal age of retirement, to see a new floor erected to make more space, and when he retired he became President of the Australian Academy of Science for a four year term. His successor was his former student, Gustav Nossal. By this time, the Hall Institute was world famous and Burnet’s contemporaries judged that Nossal would have a difficult task in matching Burnet’s record. But Nossal’s many skills were in tune with the new era of biomedical science. He possessed a formidable scientific intellect and a great appreciation of the power of new technologies. Coupled with his outgoing personality and a great gift for communication and public oratory, the stage was set for a dramatic expansion and diversification of the Institute.
In 1965, the Institute was almost entirely devoted to cellular immunology. This remained a central theme. Nossal continued his work on B cells and tolerance and brought back from England his outstanding Sydney University contemporary, Jacques Miller, to further explore the immunological significance of the thymus. Ian Mackay continued clinical research on autoimmunity initiated under Burnet. Don Metcalf, another contemporary from Sydney, was already making an international reputation in experimental haematology and this was brought into the mainstream of the Institute’s research effort. The next decade saw several additional recruitments: Thomas Mandel initiated electron microscopy and, later, transplantation biology; Noel Warner established a strong base in immunogenetics; Ken Shortman succeeded Gordon Ada and established a new tradition in cell separation; Jerry Adams and Suzanne Cory introduced molecular biology, initially to investigate antibody production and later to study the origins of cancer; Graham Mitchell initiated a vigorous program in immunoparasitology, focussed on schistosomiasis, leishmaniasis and malaria. Later, Len Harrison, Mackay’s successor, focussed the clinical group on diabetes.
Nossal realized that it was essential to broaden the funding base of the Institute, and succeeded exceedingly well in this endeavour. In 1965, 81 people worked at the Hall Institute and the recurrent expenditure was $A360,000; upon his retirement in 1996, the Hall Institute had a staff of about 320, and an annual budget of $A23 million. He also appreciated the need for state-of-the-art technology, and built up sophisticated centralized services: in mouse husbandry, mouse genetic modification, computer science, flow cytometry and protein analysis. In the early 1980s, Nossal and Sir Andrew Grimwade, then President of the Institute Board, successfully lobbied the State and Federal Governments to commit money for a new building, to be located on the northern boundary of the Royal Melbourne Hospital site. In 1985, the magnificent ultramodern Hall Institute comprising about 15,000 square metres was dedicated. It ushered in a new era of growth and increased visibility and allowed a marked expansion of the Institute’s training function, with far more postgraduate students and postdoctoral fellows. The Institute’s interface with clinical medicine at the Royal Melbourne Hospital was broadened with several joint appointments. The increased space also enabled the Institute to take part in the Cooperative Research Centre scheme, which was established to further collaborative connections between University departments, Government laboratories and industry. By 1996, the Hall Institute was the host institution for the CRC on Cellular Growth Factors, under the direction of Dr Nicos Nicola, and a partner in the CRC for Vaccine Development.
 |
| Present laboratories of the Walter and Eliza Hall Institute of Medical Research, occupied since 1985. Copyright © Walter and Eliza Hall Institute |
The intellectual accomplishments of the Nossal era were many and varied. Key contributions to cellular immunology included the discovery that T cells derived from the thymus ‘helped’ B cells to produce antibody, proof of the clonal selection theory, delineation of the earliest stages of T cell development in the thymus, and the nature of self-tolerance. The colony stimulating factors (CSFs), a new class of hormone-like growth factors which stimulate blood cell production were discovered, characterized and taken to the clinic—they have now been used to treat over 1.3 million cancer patients. A major effort was mounted to develop a malaria vaccine and the first clinical field trials are now imminent. The molecular basis of Burkitt’s lymphoma was established and the oncogene responsible for initiating follicular lymphoma was shown to regulate programmed cell death (apoptosis). Very early stages of neuronal and heart development were clarified.
Over the thirty-one years of Nossal’s directorship, the Institute went from strength to strength, still the pre-eminent medical research institute in Australia and one of the great medical research institutes of the world. In 1994 Nossal, a Fellow of the Royal Society and Foreign Associate of the US National Academy of Sciences and recipient of numerous prestigious international awards, became President of the Australian Academy of Sciences.
Nossal’s successor as Director of the Walter and Eliza Hall Institute is Suzanne Cory, also a Fellow of the Australian Academy of Science and the Royal Society and a Foreign Associate of the US National Academy of Sciences. She is a distinguished molecular biologist, known particularly for her work on antibody genes and oncogenes. The major themes of the Institute remain in place, with an increased attention on genetic predisposition to disease and bioinformatics.


G.J.V. Nossal in 1994, when he became President of the Australian Academy of Science.Susanne Cory at the age of 54, when she became Director of the Walter and Eliza Hall Institute.
Copyright © Walter and Eliza Hall Institute
Footnotes
1. Kellaway, C. H. (1928). The Walter and Eliza Hall Institute of Research in Pathology and Medicine. Medical Journal of Australia, 2, 702-708.
2. Burnet, M. (1971). The Walter and Eliza Hall Institute 1915-1965. pp. 16-42. Melbourne University Press.
3. Dale, H. H. (1953). Charles Halliley Kellaway. Obituary Notices of Fellows of the Royal Society, 8 (22), 503-521.
4. Fenner, F. J. (1987). Frank Macfarlane Burnet 1899-1985. Biographical Memoirs of Fellows of the Royal Society. 33, 113-116. Stent, G. S. (1963). Molecular Biology of Bacterial Viruses. pp. 15-16. W. H. Freeman, San Francisco.
5. Burnet, F. M. (1941). The Production of Antibodies: a Review and Theoretical Discussion. Monograph from The Walter and Eliza Hall Institute of Research in Pathology and Medicine, No 1. Macmillan, Melbourne. Burnet, F. M. and Fenner, F. (1949). The Production of Antibodies. 2nd edition. Macmillan, Melbourne.
6. Burnet, F. M. (1936). The Use of the Developing Egg in Virus Research. Medical Research Council Special Report Series No. 220. His Majesty’s Stationery Office, London.
7. Burnet, F. M. (1940). Biological Aspects of Infectious Diseases. Cambridge University Press, Cambridge.
8. Burnet, F. M. (1942). The rickettsial diseases in Australia. Medical Journal of Australia, 2, 129-134.
9. Fenner, F. (1996). Burnet’s contribution to influenza research. In Options for the Control of Influenza III. (L. E. Brown, A. W. Hampson, and R. G. Webster, eds.), pp. 3-13. Elsevier, Amsterdam.
10. Burnet, F. M. (1955). The Principles of Animal Virology. Academic Press, New York.
12. Nossal, G. J. V. (1985). The Walter and Eliza Hall Institute of Medical Research: 1915-1985. Medical Journal of Australia, 143, 153-157. Nossal, G. J. V. (1995). The Walter and Eliza Hall Institute of Medical Research 1965-1995: from basic research to clinical triumphs. Medical Journal of Australia, 163, 600-603.
Other sources of information about the Institute
Burnet, M. (1968). Changing Patterns. An Atypical Autobiography. Heinemann, Melbourne.
Burnet, M. (1971). “The Walter and Eliza Hall Institute 1915-1965.” Melbourne University Press, Melbourne.
Sexton, C. (1991). The Seeds of Time: The Life of Sir Macfarlane Burnet. Oxford University Press, Oxford.
Marchalonis, J. J. (1994). Burnet and Nossal: the impact on immunology of the Walter and Eliza Hall Institute. Quarterly Review of Biology, 69, 53-67.
Wood, I. J. (1984). Discovery and Healing in Peace and War. Acton Graphic Arts, Hawthorne.
The Walter and Eliza Hall Institute of Medical Research. Annual Review 1978-79. Special Volume: A Tribute to Sir Macfarlane Burnet. A Lifetime of Creativity. Burnet at Eighty.
Acknowledgements
Photos were kindly provided by John Wilkins, Head of Communication Services, Walter and Eliza Hall Institute.
First published 23 July 1997