Diabetes used to be a death sentence, but that changed in 1922 when a teenager’s miraculous recovery brought hope to millions. The discovery of insulin and subsequent breakthroughs by Nobel Prize laureates led to advancements in how we treat the chronic disease. Now, efforts are focused on tackling the unfolding diabetes “epidemic” and finding a cure that could relegate the disease to history.
In January 1922, a 14-year-old boy called Leonard Thompson became the first person to receive an insulin injection as a treatment for diabetes. For the first time in history, diabetes was no longer a death sentence.
Born in 1908, Leonard grew up in a working-class street in Toronto, Canada with his parents, one brother and two sisters. He was described as a happy child who loved football and other sports. However, at the age of eleven, Leonard was diagnosed with diabetes, a then incurable condition. He was put on a strict diet, which at the time was only capable of managing his symptoms.
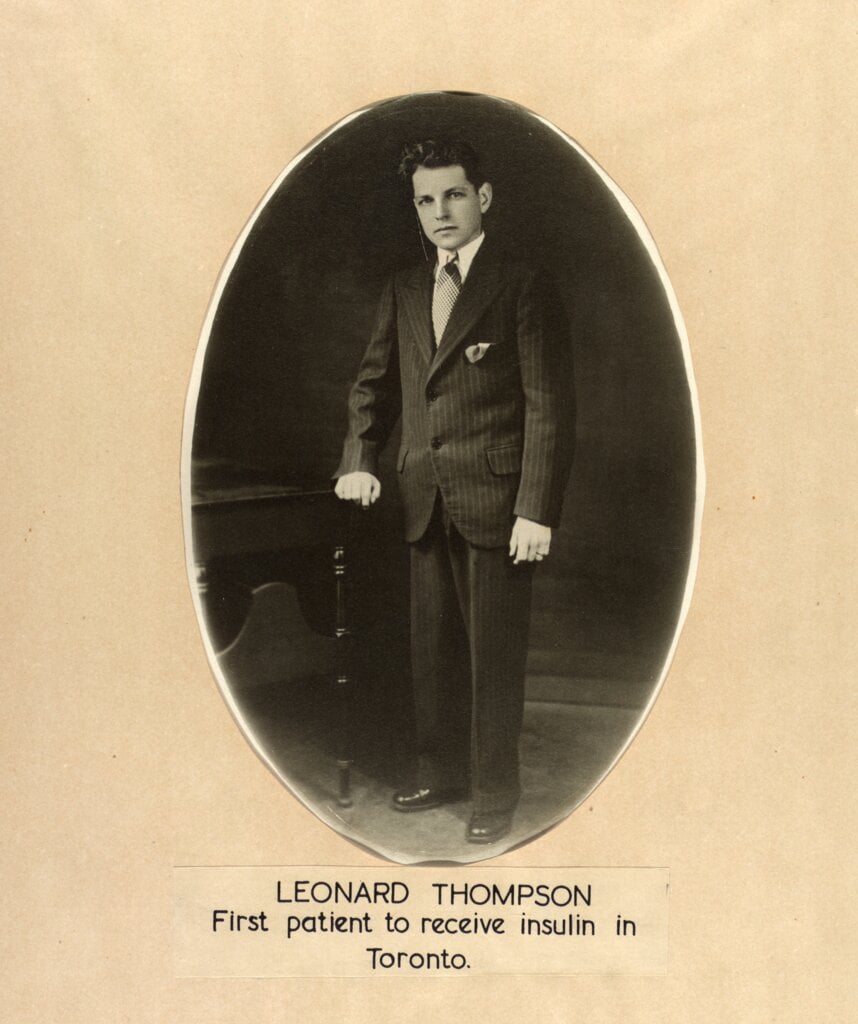
By the time he was 14 years old, Leonard was much smaller and weaker than a boy of his age should be. He weighed just 65lbs and ended up in hospital, drifting in and out of consciousness. Desperate to save their son’s life, Leonard’s parents Harry and Florence agreed for him to test a new treatment.
On January 11, 1922, Leonard received his first insulin injection. While the first attempt didn’t work, later injections showed great improvement. “The boy became brighter, more active, looked better and said he felt stronger,” according to his medical records. A few months later, Leonard had recovered enough to return home.
“It was a miracle.”
Professor Juleen Zierath, Member of the Nobel Assembly at Karolinska Institutet
Watch the video ’Insulin's impact: The story behind the 1923 Nobel Prize in Physiology or Medicine’
While Leonard was the first person with Type 1 diabetes to benefit, within just a year insulin was saving the lives of others thanks to the rapid work of researchers at the University of Toronto who managed to isolate the hormone.
More than 100 years after its discovery, insulin continues to be used to help some of the over 400 million people around the world with diabetes.
A death-defying discovery
Diabetes is a chronic disease that occurs when a person’s blood sugar is too high. Long before the discovery of insulin, doctors suspected that the pancreas secreted a substance that controlled carbohydrate metabolism. During the beginning of the 20th century, several attempts were made at preparing pancreatic extracts that could lower blood glucose. However, due to an inability to remove impurities, toxic reactions prevented its use in humans.
In the early 1920s, a young surgeon called Frederick Banting came up with an idea to solve the diabetes enigma. Reportedly waking up in the middle of the night, he scribbled down his hypothesis on a piece of paper.
For Banting the key was isolating a pure version of pancreatic extract that could be used to treat diabetes. His breakthrough was hypothesising that another substance produced in the pancreas, trypsin, was breaking down insulin before it could be extracted. He set about trying to overcome this problem.
Banting reached out to John Macleod, professor of physiology and department head at the University of Toronto. In John Macleod’s laboratory in 1921, Frederick Banting and his research assistant Charles Best treated dogs so that they no longer produced trypsin. Insulin could then be extracted and used to treat diabetes. When they managed to isolate insulin from dogs, colleagues remarked that it looked like “thick brown muck”. Biochemist James Collip joined the group to work on purifying insulin so it would be safe enough to be tested in humans, and together they refined the substance so that it could give hope to Leonard Thompson and countless others with diabetes.
Banting, Collip and Best were awarded US patents on insulin and the method used to make it, but sold them to the University of Toronto for $1 each.
“Insulin does not belong to me, it belongs to the world.”
Frederick Banting
Demand for insulin surged as news of Leonard’s remarkable recovery spread.
“One by one the implacable enemies of man, the diseases which seek his destruction, are overcome by science. Diabetes, one of the most dreaded, is the latest to succumb,” said an article in The New York Times.
The researchers refined their production techniques so the wonder-treatment could be produced in larger quantities, and in October 1923 the first commercial supply of insulin was shipped.
In the same month, Banting and Macleod were awarded the Nobel Prize in Physiology or Medicine 1923. However, they were unhappy that the important contributions of their collaborators had not been recognised, so the laureates shared the prize money with Best and Collip.
A new dawn for diabetes
“Since then, the understanding of how insulin works has exploded,” says Anna Krook, Professor at the Karolinska Institutet. Its discovery kickstarted a flurry of research that led to even more scientists receiving Nobel Prizes.
Frederick Sanger was one of them, awarded the Nobel Prize in Chemistry 1958 “for his work on the structure of proteins, especially that of insulin.” He began studying the composition of the insulin molecule in the 1940s, using acids to break the molecule into smaller parts, which were separated from one another with the help of electrophoresis and chromatography. Further analyses determined the amino acid sequences in the molecule’s two chains, and in 1955 Sanger identified how the chains of 51 amino acids are linked together.
This was a huge achievement and the first time that the structure of a protein had been determined.
Another method – X-ray crystallography – enabled 1964 chemistry laureate Dorothy Hodgkin to “see” the structure of insulin molecules for the first time. She began investigating the 3D structure of insulin at the age of 24, pausing her work to take on penicillin, which was a more urgent task in the World War II era. After 34 years of research, Dorothy Hodgkin was able to map the structure of insulin, shedding more light on the intriguing hormone.
Sanger’s work, followed by Hodgkin’s 1969 discovery of the 3D shape of insulin, paved the way for scientists to be able to produce man-made insulin in the lab, which millions of people with diabetes use today.
Ten years before Hodgkin mapped insulin, another laureate made a breakthrough that would also revolutionise the treatment of diabetes. Together with her research partner Solomon Berson, 1977 medicine laureate Rosalyn Yalow made a transformative contribution to medical research: radioimmunoassay (RIA), a method for measuring concentrations of substances in the blood.
The pair first attempted to use radioisotopes to more accurately estimate blood volume and soon applied their methods to insulin, in part because Yalow’s husband was diabetic.
Yalow and Berson attached radioactive iodine to molecules of insulin and injected minute amounts of the radioactive-tagged insulin into volunteers, including themselves. Blood samples taken over several hours showed how quickly the insulin was being metabolised. Using this technique, they found that people with Type 2 diabetes were unable to process insulin not because they lacked the hormone, but because their bodies produced an antibody that rejected it. This was a big discovery for the treatment of diabetes.
As a result of Yalow’s work, many diseases and conditions including diabetes can be diagnosed, treated, or tested. RIA is so sensitive that it can detect a teaspoonful of sugar in a body of water 62 miles long. Tens if not hundreds of millions of radioimmunoassays are made annually in hospitals to measure hormones such as insulin with just a drop of blood, enabling people with diabetes to receive treatment as quickly as possible.
Fighting an unfolding “epidemic”
Today, quicker diagnosis is important, as more people than ever are being diagnosed with diabetes. Insulin continues to be the treatment of choice and is available in many forms, from a synthetic hormone identical to the one produced in the pancreas, to ultra-rapid and ultra-long-acting insulins, enabling people with access to insulin who have Type 1 diabetes, to have a life expectancy approaching that of non-diabetics.

But there’s a growing challenge, spurring the need for new treatments. Today, more than 95 percent of people with diabetes have Type 2 diabetes. Related to obesity, which is due to changes in diet and lifestyle, it is still on the rise, posing a major threat to human lifespan and health span.
Some experts have warned it is an “epidemic” and it’s driving the need for more research. Weight loss plans and beta cell transplants using lab-grown cells are being explored to try and help people with Type 2 diabetes regain normal blood glucose levels. One hope is that drugs or gene deliveries could one day “tweak muscle” to respond better to insulin if people are not getting enough exercise, Professor Anna Krook of the Karolinska Institutet explains.
New treatments for Type 1 diabetes may also be on the horizon. Researchers are developing and testing immunotherapies that target the immune system to stop it from destroying beta cells in the pancreas that produce insulin. If they succeed, immunotherapies could one day prevent people from developing Type 1 diabetes at all.
The revolutionary discovery by Frederick Banting and his co-workers have paved the way for the next generation of research into diabetes. According to Professor Juleen Zierath of the Karolinska Institutet, a definite solution to end the diabetes epidemic is possible: “I’m really hopeful that researchers will come closer to finding a cure for diabetes and I believe that we have great tools in our hands.”
This article was published on 13 November 2024.